A nurse is more than a caregiver. You’re often the steady compass guiding patients through some of life’s stormiest health challenges. And when it comes to obesity, the journey can feel like an uphill climb in a headwind.
That’s where your role becomes especially powerful. Patients struggling with obesity need more than prescriptions. They need perspective and encouragement. Whether you’re helping someone build confidence with small lifestyle changes or supporting semaglutide weight loss with ongoing nurse support, your presence can shift the course of a patient’s health journey for good!
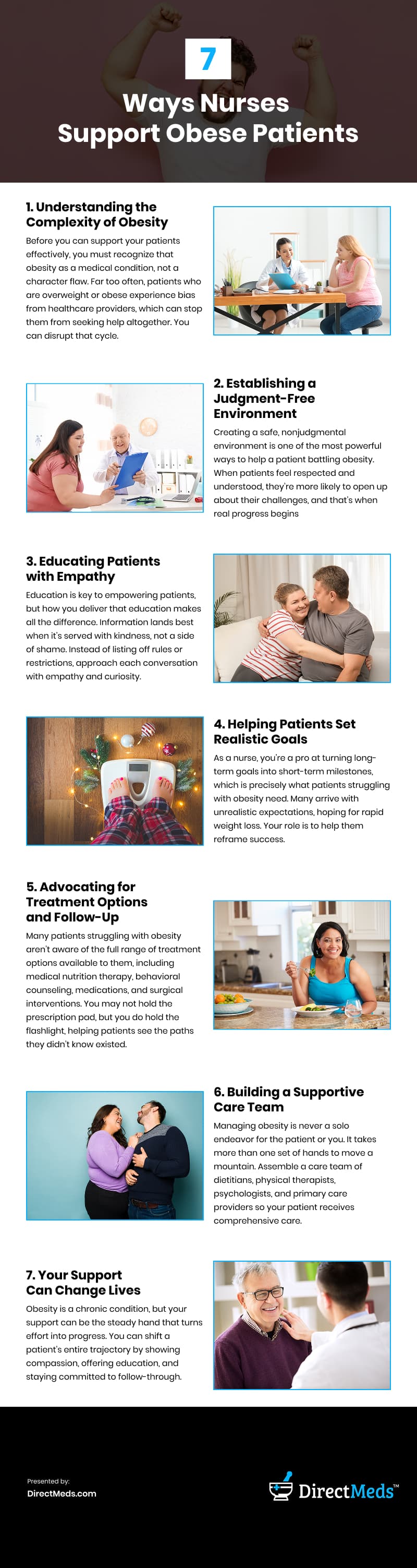
Understanding the Complexity of Obesity
Before you can support your patients effectively, you must recognize that obesity as a medical condition, not a character flaw. Far too often, patients who are overweight or obese experience bias from healthcare providers, which can stop them from seeking help altogether. You can disrupt that cycle.
When you understand the multifaceted nature of obesity, your patient care becomes more holistic. Genetics may predispose someone to gain weight easily. Emotional trauma can lead to using food as a coping mechanism. Chronic stress, lack of access to healthy food, and sedentary work environments all add layers to the issue. Understanding obesity means shifting the focus from blame to biology, and that’s a change patients can feel from the inside out.
The more you acknowledge the science behind obesity, the more effective and empathetic your care becomes. Validate your patient’s struggles and open the door to practical, sustainable interventions that go beyond “just eat less and move more.”
Establishing a Judgment-Free Environment
Creating a safe, nonjudgmental environment is one of the most powerful ways to help a patient battling obesity. When patients feel respected and understood, they’re more likely to open up about their challenges, and that’s when real progress begins.
It starts with simple but impactful actions that build trust and reduce shame. Keep these tips in mind:
- Use respectful language
- Maintain neutral facial expressions during weight discussions
- Avoid terms that carry stigma
- Replace phrases like “morbidly obese” with “person with obesity.”
By changing conversations around obesity you can build a therapeutic alliance where the patient feels like a partner, not a problem.
Educating Patients with Empathy
Education is key to empowering patients, but how you deliver that education makes all the difference. Information lands best when it’s served with kindness, not a side of shame.
Instead of listing off rules or restrictions, approach each conversation with empathy and curiosity. Ask open-ended questions to learn what your patient already understands about nutrition and weight management. Then, fill the gaps with guidance tailored to their needs and lifestyle.
Explain how their online GLP-1 weight loss prescription will affect their metabolism or how sleep deprivation contributes to weight gain. Perhaps your patient doesn’t realize that high cortisol levels from chronic stress can cause fat retention.
A good nurse hands out more than facts. They translate the science into something patients can use in their lives. When you break it down in an accessible way, you give your patients the tools they need to make informed choices without feeling overwhelmed.
You’re not just a nurse. You’re a coach, an advocate, and a cheerleader for their health journey.
Helping Patients Set Realistic Goals
As a nurse, you’re a pro at turning long-term goals into short-term milestones, which is precisely what patients struggling with obesity need. Many arrive with unrealistic expectations, hoping for rapid weight loss. Your role is to help them reframe success.
Explain that every small win is like adding a brick to a stronger foundation. Even modest weight loss—just five to ten percent of their body weight—can significantly improve blood pressure, cholesterol, and insulin sensitivity. When you celebrate these smaller victories, you shift the focus from the number on the scale to their progress in health and quality of life.
Here are a few ways to guide goal-setting effectively:
- Encourage SMART Goals: Help your patient set Specific, Measurable, Achievable, Relevant, and Time-bound goals. For instance, “walk 15 minutes a day, five times a week” is more actionable than “start exercising.”
- Normalize Setbacks: Make sure they understand that plateaus and regressions are normal. Your encouragement during these phases can keep them from giving up.
- Focus on Non-scale Wins: Highlight improvements like increased energy, better sleep, or reduced joint pain as equally important to weight metrics.
Advocating for Treatment Options and Follow-Up
Many patients struggling with obesity aren’t aware of the full range of treatment options available to them, including medical nutrition therapy, behavioral counseling, medications, and surgical interventions. You may not hold the prescription pad, but you do hold the flashlight, helping patients see the paths they didn’t know existed.
You can make valuable referrals and advocate for comprehensive care in the clinical setting. Explain the options and guide your patient through questions they may want to ask during follow-up visits with their provider.
Follow-up is critical. Obesity treatment is not a one-and-done chat. It’s more like a book club. Keep showing up for the next chapter. It’s a long-term process that requires ongoing support. Schedule regular check-ins, monitor progress, and continue educating to create a sense of continuity that improves outcomes.
Building a Supportive Care Team
Managing obesity is never a solo endeavor for the patient or you. It takes more than one set of hands to move a mountain. Assemble a care team of dietitians, physical therapists, psychologists, and primary care providers so your patient receives comprehensive care.
Facilitate communication between collaborators and advocate for your patient’s needs. Healing happens faster when everyone’s rowing in the same direction. Connect patients to local resources such as support groups or community wellness programs, offering guidance outside clinic walls. You’re the thread that ties their care plan together.
Your Support Can Change Lives
Obesity is a chronic condition, but your support can be the steady hand that turns effort into progress. You can shift a patient’s entire trajectory by showing compassion, offering education, and staying committed to follow-through.
You aren’t just helping someone lose weight. You’re helping give them a renewed sense of hope. And that impact? It lasts far longer than any treatment plan ever could.
Video

Infographic
Nurses play a vital role in supporting patients on their journey to manage obesity. Beyond administering prescriptions and monitoring vital signs, they offer encouragement and foster trust. This infographic highlights the meaningful ways nurses assist individuals facing obesity.